
News
Facing the Hidden Crisis: Maternal Suicide in the U.S.
Maternal suicide is an often overlooked yet leading cause of death in the perinatal period—especially during the first year after childbirth. Despite this, it has historically been undercounted or excluded in maternal mortality data, which has contributed to gaps in awareness and prevention efforts. New research from Maternal Mortality Review Committees shows that mental health conditions contribute to nearly a quarter of pregnancy‑related deaths, with suicide making up about 30%. These findings highlight the urgent need for comprehensive mental health care to be a core component of maternal health services.
Risk factors for maternal suicide are complex and multi‑layered, often involving a combination of past psychiatric illness, depression or anxiety, substance use disorder, and trauma. Social determinants such as lack of social support, financial or housing stress, abuse, and systemic inequities further compound these risks. Importantly, most maternal suicides occur between six weeks and a year postpartum—after the standard six-week postpartum follow-up appointment—underscoring the urgent need for care that extends well beyond childbirth. This extended vulnerability period calls for ongoing screening, support, and accessible resources to protect birthing individuals during this critical time.
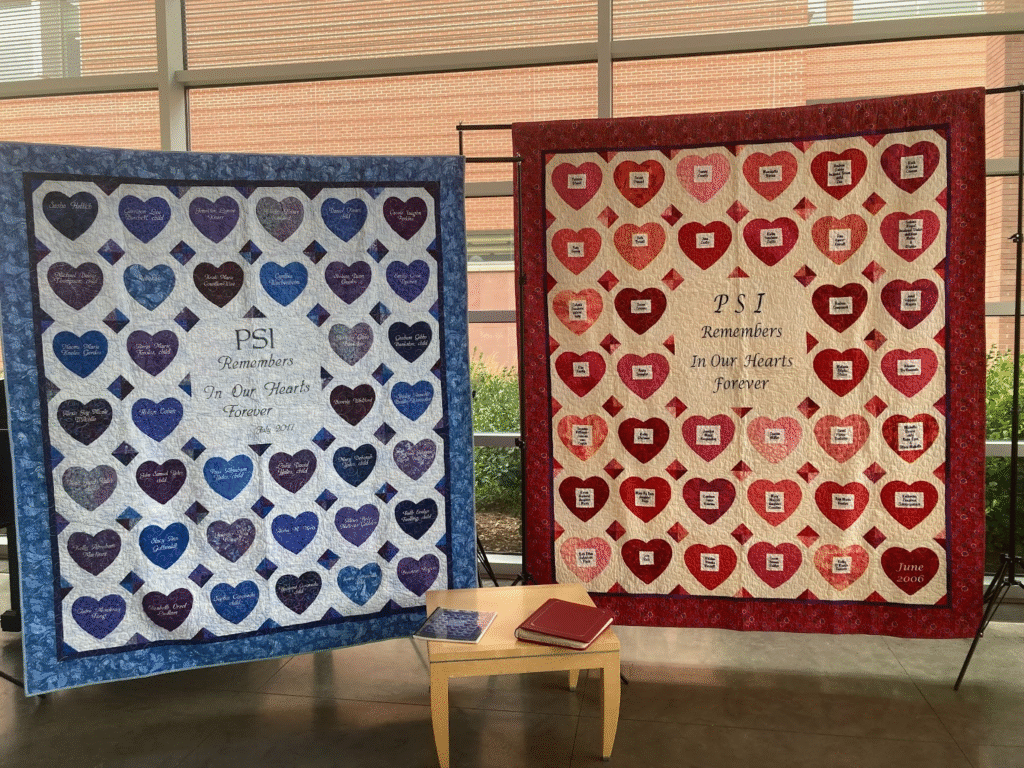
The Postpartum Support International (PSI) Memorial Quilt honors mothers and infants who have died from postpartum mood disorders (PMADs). Photo taken at the September 2025 National Convening on Maternal Suicide Prevention hosted by University of Colorado School of Medicine
Taking Action to Prevent Maternal Suicide in Colorado
In Colorado, suicide was the leading cause of maternal death between 2016 and 2020. Pregnant and postpartum individuals were found to be more than twice as likely to die by suicide compared to the general population of reproductive-age women. The Colorado Maternal Mortality Review Committee (MMRC) determined that 100% of these deaths were preventable—meaning that with the right support, interventions, and systemic changes at the patient, provider, community, or policy level, lives could have been saved.
Responding to this urgent need, CPCQC is taking action through programs like IMPACT BH, which integrates behavioral health into perinatal care; SPARK, which supports the critical transition from hospital to home; and Turning the Tide, which improves substance use screening and peer support in hospitals. These efforts reflect CPCQC’s commitment to saving lives and supporting families statewide.
Building on this momentum, CPCQC participated in a two-day hybrid National Convening on Maternal Suicide, hosted by the University of Colorado School of Medicine. The event brought together individuals with lived experience, researchers, clinicians, advocates, and policymakers to collaboratively shape the future of research aimed at preventing perinatal suicide. Together, attendees co-developed a roadmap for patient-centered outcomes research, focusing on strategies including resource mapping, provider training, prevention efforts, and building stronger support networks. This convening marked an important step forward, as CPCQC and partners launched new efforts to collectively address and reduce perinatal suicide across the country.

Photo of attendees at the September 2025 National Convening on Maternal Suicide Prevention. Attendees included but were not limited to Postpartum Support International, the Maternal Mental Health Leadership Alliance, and the Policy Center for Maternal Mental Health
As awareness grows and collaborative efforts expand, CPCQC remains dedicated to advancing maternal mental health and preventing perinatal suicide in Colorado and beyond. By integrating evidence-based programs, fostering partnerships, and amplifying the voices of those with lived experience, we can create a system of care that truly supports every perinatal family.
Recognizing signs of perinatal suicide and psychosis is critical. Some warning signs include prolonged feelings of hopelessness or guilt, withdrawal from family or friends, mood swings, talking about death or suicide, or loss of interest in caring for the baby. Postpartum psychosis may include hallucinations, delusions, severe confusion, or thoughts of harming self or baby, and is a medical emergency.
If you or someone you care about is struggling, help is available 24/7. The National Maternal Mental Health Hotline (1‑833‑943‑5746) offers free, confidential support. You can also call or text 988 to reach the Suicide & Crisis Lifeline. Postpartum Support International provides peer support, provider referrals, and groups via postpartum.net.
Keep Reading


Our Primary Cesarean Program is Planning a Re-launch in 2024

